The hidden abuse of chemsex: ‘It’s like connecting on the edge of the abyss’ Problematic substance use leads to relational difficulties, mental health issues, and addiction, which, in the worst cases, can result in overdose deaths or suicide Chemsex has always navigated a web of silence — caught between stigma and serious health risks. It refers to the intentional use of drugs to sustain sexual activity over extended periods, and is primarily practiced among men who have sex with men (MSM). It is a high-risk practice — linked to an increased likelihood of contracting sexually transmitted infections (STIs) and the use of potentially addictive substances — but it has also become a way of socializing.
A dozen experts consulted agree that chemsex is a minority practice — prevalence rates vary widely from 3% to 30% , depending on the study — though one that is clearly on the rise. Most individuals who engage in chemsex do so recreationally, without it becoming a life-threatening issue. However, experts warn that a significant, albeit hard to quantify, proportion develops problematic use — yet there is still no adequate health infrastructure or sexual-affective support to meet their needs.

Problematic chemsex use often manifests through strained relationships, mental health disorders, and addiction — sometimes escalating to fatal outcomes such as overdose or suicide. Activists and experts have long sounded the alarm about the far-reaching consequences of such use, and, most urgently, the glaring lack of resources and comprehensive strategies to effectively address these situations. They warn of the invisibility of a complex and often overlooked issue, exposing the wide range of harms that can arise when chemsex spirals out of control.
One of the primary concerns is addiction to substances commonly linked to the practice — such as methamphetamine , GHB (also known as liquid ecstasy), cocaine, and mephedrone. In clinics and community centers, mental health problems stemming from the abuse of these substances is increasingly evident, with cases of paranoia, psychotic episodes, depression, anxiety, and a growing inability to engage in sex without the aid of drugs. Toni Gata, a psychologist at the BCN Checkpoint community center, has been seeing the dark side of chemsex for years.
In 2024 alone, 340 new clients sought help for related issues. “The problem today is nothing like what we saw in 2017. Back then, injecting was rare.
Now, more than half have injected at some point, and that brings much more serious complications. Since 2022, we’ve been seeing a surge in psychotic disorders and delirium — one or two new cases every day,” he says. In response, the center has added a psychiatric service specifically to manage these symptoms.
Regarding the worst-case scenario — deaths — there is no data, only hearsay and word of mouth. Jorge García, head of the Drassanes-Vall d’Hebron STI unit, explains: “We don’t know the number of people who may be dying from chemsex. What we’re seeing here are long-term problems with methamphetamine use, which can lead to suicidal thoughts, or the most acute problem, GHB overdoses.
” In any case, attributing a death directly to chemsex is challenging, as it is a complex phenomenon intertwined with a range of life circumstances that independently carry health risks. “The deaths of users are multifactorial; they can occur during the sessions themselves, from overdoses or suicide, but other factors may be at play, such as the individual’s structural condition or mental health issues,” says Ovi Leonarte, activist and spokesperson for the Alliance for Freedom and Psychoactive and Human Ethics platform. The scientific literature is peppered with case reports that shed light on some extreme situations of problematic chemsex use: in 2017, for example, a British study warned of a rise in deaths from GHB overdoses, linking it, in part, to chemsex; in 2021, another review in France recorded 13 poisonings related to this phenomenon, six of them fatal.
Emilio Salgado, head of Clinical Toxicology at the Hospital Clínic in Barcelona, admits that “it’s difficult to associate a toxic substance with this practice,” but the cases most often associated with it are GHB poisonings. The hospital sees about five a week, although Salgado says they cannot confirm that all are related to chemsex. What he can confirm is that these numbers have remained stable and have not shown an upward trend in recent years.
“Both drugs and sex are two powers and come with a great responsibility,” says Sandro Bedini, 49, regarding his relationship with chemsex. He began exploring the scene more than a decade ago, initially without drugs, drawn by the desire to experiment sexually within that context. Over time, however, substance use entered the picture and eventually overshadowed everything else in his life.
“There’s an initial phase, called the honeymoon, where you socialize very successfully and enjoy yourself a lot. Then, I went through a long phase of denial, where things happen around you that get out of hand, but you deny it. It’s gradual: you arrive late to work, you lose responsibilities, life plans you once had are eroded, your free time is focused on chill [the colloquial term for chemsex encounters].
The transition from denial to acknowledging that you have a problem is a mystery: you give up when it’s no longer worth it,” he reflects. Before reaching that point, he admits, there’s a long journey through walls of silence, built in his case by “guilt” and an inability to “recognize one’s own vulnerability.” To understand chemsex — particularly its progression into problematic use — it’s essential to place the phenomenon within the broader context of a community that has often experienced its sexuality through the lens of discrimination and heteronormativity.
Experts point to a range of cultural factors that have shaped its development: global taboos around sex, the experience of masculinity, the lasting stigma of the HIV pandemic, societal pressures around body image, and the rise of dating apps. As a result, chemsex can serve multiple purposes. It may be used to enhance libido and pleasure, lower inhibitions, or explore specific sexual fantasies .
At the same time, it can also mask fear of rejection, loneliness, low self-esteem, or internalized homophobia. For García, the greatest risk lies in using these practices “to avoid negative sensations.” “They can be used hedonically, for the positive effect and through good mental health management.
But if the intention is to avoid all the harm that has been done to you in your life through abuse, discrimination, and stigma, then the person is using these substances to escape, which makes them feel more necessary and ultimately creates even more problems.” Emilio, 63, also a chemsex user, considers this practice “a way of connecting the edge of the abyss”: “You can either fall into it or not.” It exists in a space between pleasure and danger.
“You get hooked on the type of sex before you get hooked on the substance. You get used to an intensity that has nothing to do without substances in between,” he adds. But things can change, and what begins as a social activity can end up being something more than an addiction, he admits.
“It starts out as a way of connecting, and if it gets out of hand, it gets very complicated.” There are several risk factors that predispose individuals to problematic chemsex use. These include a history of traumatic experiences, lack of social support networks (migrants are particularly vulnerable), and pre-existing mental health issues.
The substances themselves — some of which have a higher addictive potential — and the method of administration also play a significant role. For instance, injection (or “slamming”) carries an elevated risk The dynamics of chemsex abuse operate like an intricate network, where individual factors and social context are deeply intertwined. García gives a couple of examples: “It depends on the substances being sold.
Mephedrone is illegal, and we’re seeing the emergence of other synthetic cathinones [stimulants known as ‘bath salts’] with shorter half-lives, which require repeated dosing and more easily lead to addiction. Then there are also psychobiographical factors: the LGBTQ+ population already starts from a baseline of compromised mental health due to stigma and developmental challenges in childhood and adolescence within a society where the norm is to be cisgender and heterosexual. For example, 20% of the MSM population experience mental health issues, even without factoring in chemsex.
” Alberto Díaz Santiago, a doctor in the HIV, STI, and PrEP Unit of Internal Medicine at Puerta de Hierro Hospital in Madrid, warns that any drug use can be problematic: “It’s a fine line.” Some red flags for the specialist include “when use stops being occasional, if there has been an overdose, or if drugs are being used intravenously.” He also points to signs of “disruption” in daily life: quitting work, skipping meals or family gatherings, shrinking one’s social circle to only those who use drugs, becoming isolated.
.. Díaz Santiago and García agree on a guiding question to help gauge whether drug use may be problematic: “When was the last time you remember having sex without drugs involved?” “I believe use becomes problematic when there’s an activity that involves drugs and you can’t do it without them,” García explains.
Even so, in order to gain awareness of the problem and ask for help, one must break through multiple layers of silence that help keep high-risk situations invisible. One such layer lies between those affected and a healthcare system that often feels hostile. “Public health services are heteronormative.
You go to the doctor and they assume you’re heterosexual. There’s a lot of homophobia. Sexual diversity is not present,” says Leonarte, who also denounces “police crackdowns” on chemsex in gay clubs and saunas.
García reflects on the meaning of staying silent: “Silence within the LGBTQ+ community when it comes to discussing issues that affect them — whether related to sexual practices or substance use — is not a silence that stems from stigma or shame. It’s a defensive strategy against certain sectors of society that are just waiting for an excuse to attack dissident and non-normative behaviors.” All sources agree that a supportive, trusting, and empathetic environment is essential for someone struggling with these issues to recognize their situation and consider seeking help.
Eva Orviz, clinical director of Sandoval II and coordinator of the STI centers at Sandoval in Madrid, stresses the importance of “always keeping the door open” to consultations: “The key lies in prevention, support, and avoiding stigmatization.” The care response, in any case, is faltering on all fronts. There is a lack of welcoming, safe support systems free of stigma and discrimination.
And when care is available, it often involves referring individuals to traditional drug dependency services — without addressing the relational, emotional, and psychosocial layers that are deeply entwined with chemsex. Luz Martín Carbonero, spokesperson for the AIDS Study Group (Gesida) of the Spanish Society of Infectious Diseases and Clinical Microbiology, points out that her greatest concern is “the problem of addiction and everything that entails for affective-sexual health.” “It takes its toll on them because sex without drugs is no longer satisfying, and they can’t have relationships without using,” she says.
But this isn’t solved by treating the addiction alone. “Addiction ends up being the symptom of a problem. The approach that has been taken is to focus on the drug as a problem, but the focus has to be on the person, on their context,” says Jordi Garo, head of the Chemsafe project at Energy Control.
The breakdown in care occurs “on multiple levels,” acknowledges Díaz de Santiago: “There are no psychological support points in hospitals, and psychiatrists aren’t used to treating chemsex. Mental health centers have huge waiting lists, and while addiction centers work well, not all patients feel comfortable there.” What doesn’t help, experts insist, is simply walking away: distancing oneself from the chemsex scene without pairing that decision with therapy to explore the underlying issues behind the problematic use.
NGOs have stepped in to fill the gaps left by the public system, but they’re also overwhelmed. Luis Villegas, director of the NGO Stop, says they currently have 16 people on their waiting list for intake programs: “Addiction centers don’t address the complexity of chemsex. The only way to act is through cooperation.
There’s no other option.” Joan Ramon Villalbí, the Spanish government’s delegate for the National Plan on Drugs, acknowledges the addictive potential of certain substances in these contexts, but advocates for a different approach: “inform, don’t criminalize.” “We’re concerned, we’ve made it a priority, and we’re following it closely.
Ideally, we need to create well-coordinated care networks in collaboration with the third sector. We will have to find ways to make services welcoming and accessible,” he says. Bedini went through NGO Stop’s intake services, attended therapy, and eventually left Barcelona to distance himself from the chemsex social circle.
It’s been over a year since he left addiction behind, and now, back in Barcelona, he’s testing himself and his relationship with the practice: “I have to stay vigilant. Now I’m asking myself if I want to use for recreation or as an escape. If it’s to escape, I see it as a relapse.
But even if it’s responsible use, by choice, I still don’t feel like I enjoy it as much as before, because I have something anchored there. The conclusion is that these experiences are becoming more and more spaced out because after everything I’ve been through, I no longer enjoy it, and because I’ve become aware of how getting high usurps the genuine power of enjoyment from sex.” He now volunteers at NGO Stop’s intake network and shares a positive message: “If anyone reading this is going through a difficult time with substance abuse problems, they should know that you can leave this behind, change, and feel the joy of life again.
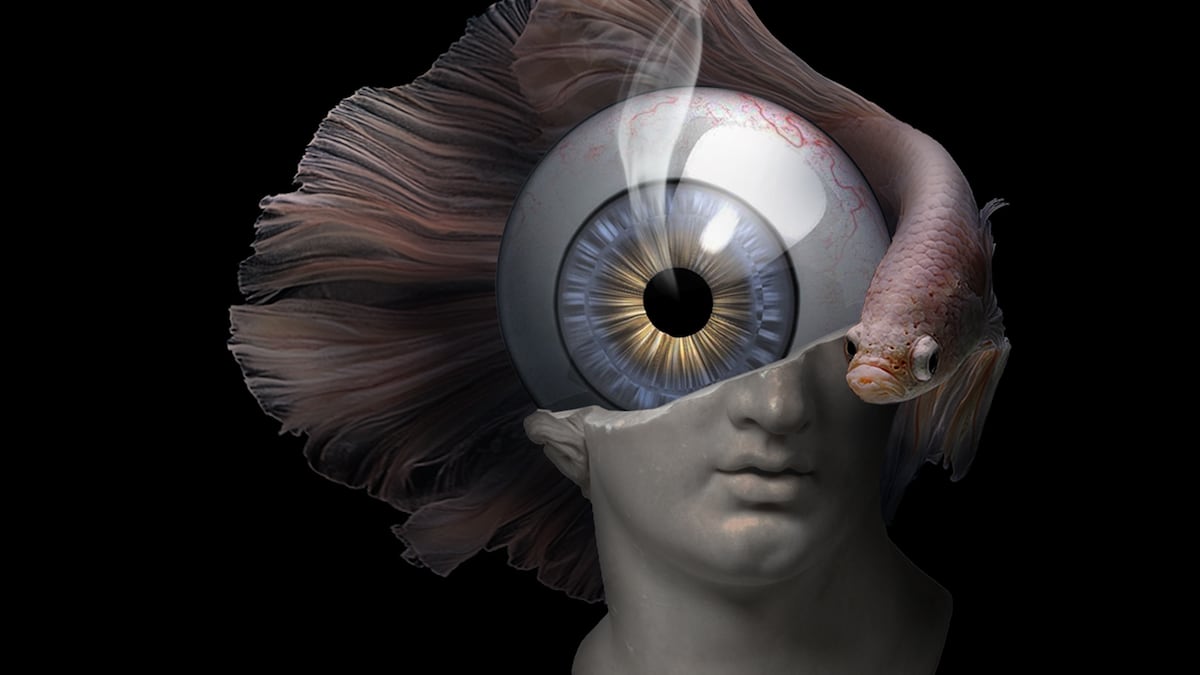
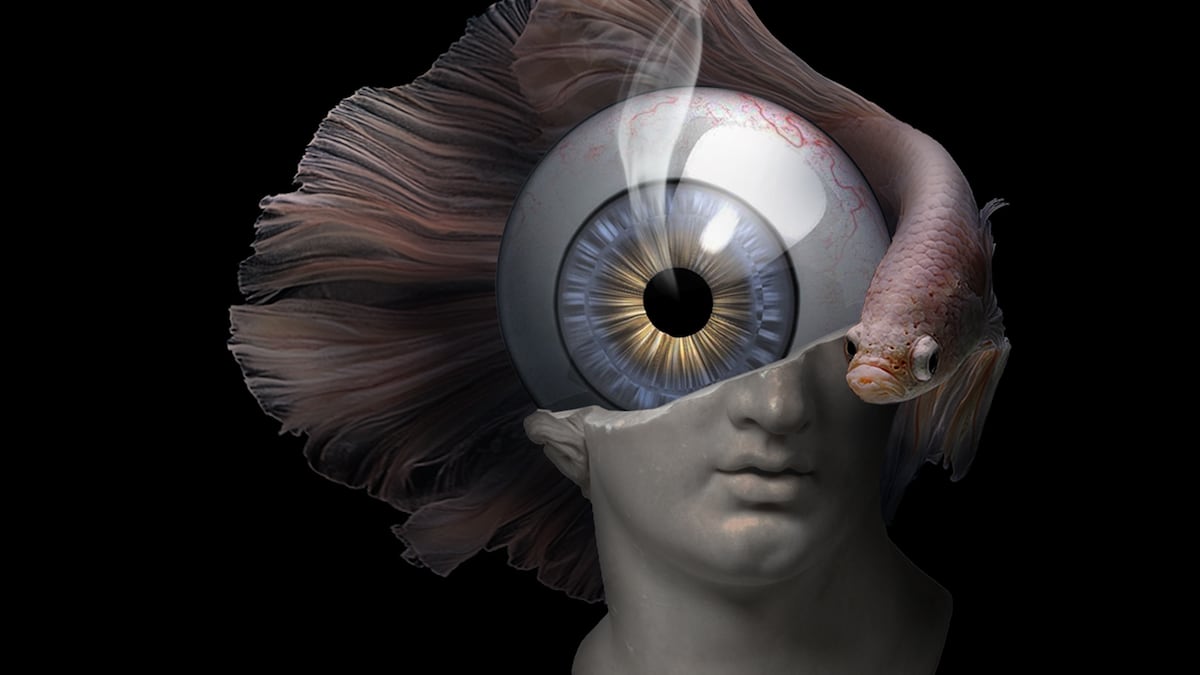
” This feature is illustrated by a visual composition created by Sandro Bedini during his therapeutic process to address problematic chemsex use and his methamphetamine addiction. He explains that the piece emerged intuitively, without a specific intention, but the act of creating it became a kind of “bridge” that helped him understand his inner world. Four years after conceiving it, now recovered, he interprets the lidless eye as a “symbol of the hyper-vigilance” brought on by meth use and “the relentless judgment you subject yourself to.
” He describes the smoke, reminiscent of that from a pipe used to inhale the drug, as “a sign of the fire” that dwells within him. And in the fractured, lifeless sculpture, he now recognizes “the fragmentation of one's own identity” and the inner conflict. “The composition is isolated and without context, much like the darkness you can end up living in when you're hooked," he reflects.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition Tu suscripción se está usando en otro dispositivo ¿Quieres añadir otro usuario a tu suscripción? Si continúas leyendo en este dispositivo, no se podrá leer en el otro. ¿Por qué estás viendo esto? Tu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez. Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario.
Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS. ¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas. En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital. Paranoia Barcelona World leaders and faithful bid farewell to Pope Francis as the Church prepares to choose his successor Living like a nobleman: The highly profitable trend of restoring historic buildings When Pope Francis was Jorge Bergoglio: An uncomfortable archbishop in Buenos Aires The trans women who sat with Pope Francis: ‘He told me not to lose faith, because we are all equal in the eyes of God’ The corrupt Pope who sold his office for money and forced the Church to create the conclave NASA astronaut Kathryn Thornton: ‘All the progress we’ve made over the past 70 years is in peril’ Who’s who in the conclave: The 133 cardinals who will elect the new pope Son of a CIA deputy director fought and died in Ukraine as a Russian soldier Traditionalists who tried to overthrow Pope Francis wait for their moment at the conclave.
Top
The hidden abuse of chemsex: ‘It’s like connecting on the edge of the abyss’
Problematic substance use leads to relational difficulties, mental health issues, and addiction, which, in the worst cases, can result in overdose deaths or suicide











